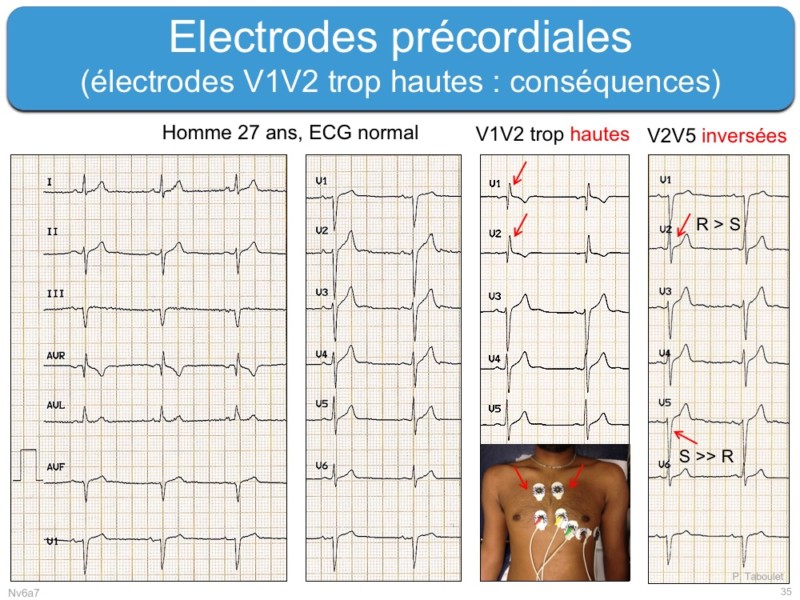
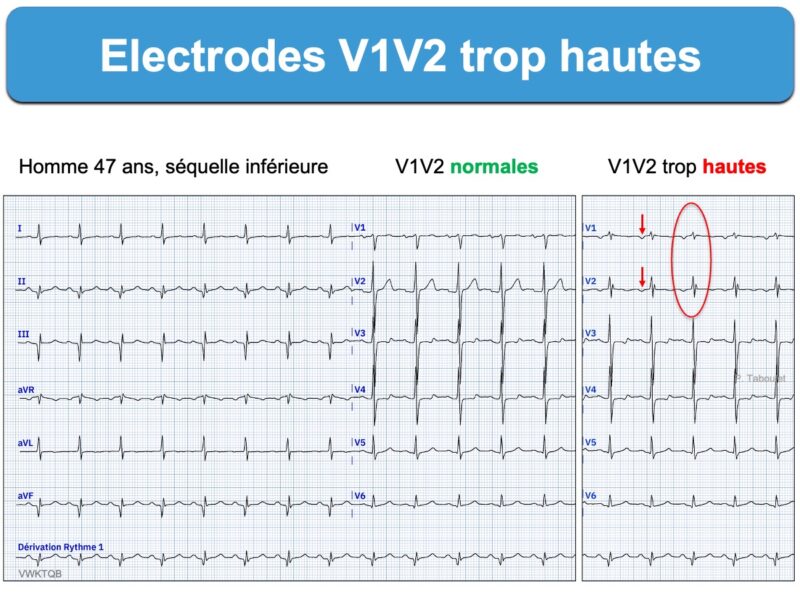
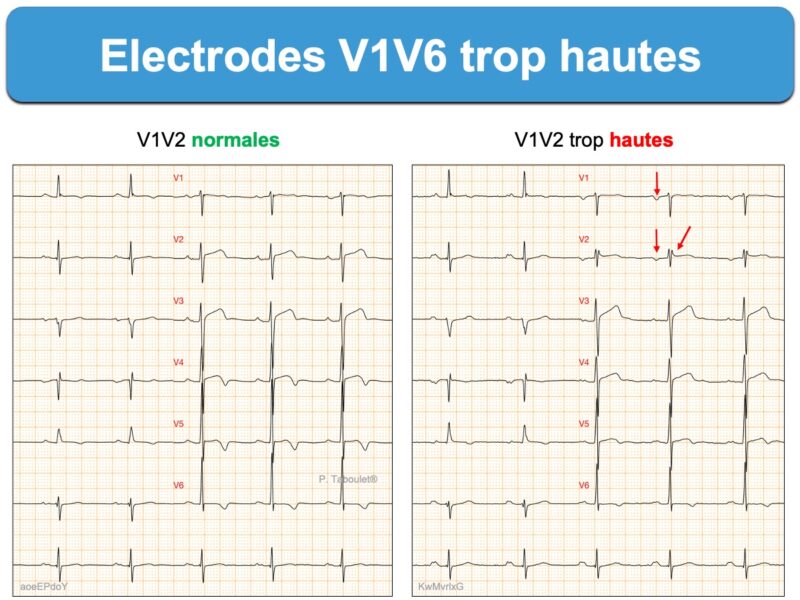
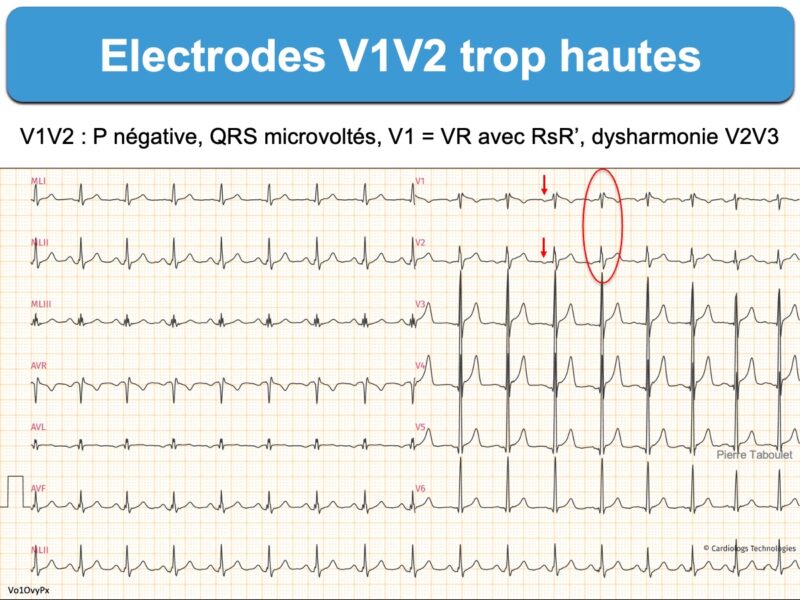
Erreurs fréquentes dans la pose des électrodes précordiales qui génèrent des erreurs d’interprétation et de reproductibilité [1][2][3] :
- faux bloc incomplet droit
- fausse hypertrophie atriale gauche
- faux ST+ ou faux “Brugada” (aspect du ST-T en selle de cheval)
- fausse onde Q de nécrose (Why is there ST Elevation in lead V2? Think Lead Placement)
- microvoltage masquant une HVG
- anomalie de repolarisation (masquée ou ajoutée, ex. T négative en V2)
Vidéo. P. Taboulet. Comment enregistrer un ECG
Vidéo. P. Taboulet. Séquelle d’infarctus septal ?
Repérage de V1V2 trop hautes
Anomalies évocatrices possibles en V1V2
- ondes P à prédominance négative
- onde R’ en V1 ou V2 simulant un bloc incomplet droit
- complexes QRS plus petits que V3 V4, ou QR simulant une séquelle de nécrose [2][4]
- V1 ressemble parfaitement à VR (deux dérivations supéro-droites), ce qui doit donner l’alarme.
Rappel technique
Il faut poser les électrodes V1-V2 au 4e espace intercostal. Pour cela, il faut :
- repérer l’Angle de Louis (qui identifie l’insertion des 2èmes côtes sur le sternum) [5]
- ou (ma méthode) positionner en premier l’électrode V4 dans le sillon sous mammaire gauche sur la ligne médio-claviculaire (fossette palpable avec l’index), puis poser V2 en parasternal gauche, 1 espace intercostal plus haut, puis poser V1 en parasternal droite en regard de V2, puis V3 exactement entre V2 et V4 et on poursuit avec V5 et V6 sur la même ligne que V4 (cf. Electrodes précordiales) [6].
Une aide au repérage du mauvais positionnement des électrodes par les algorithmes d’interprétation ou “machine learning” est possible [7].
7 références commentées (réservées aux abonnés)
La suite est réservée aux membres et stagiaires du site.
Connexion | Devenir membre | Devenir stagiaire